How does compression help after surgery?
The patient's well-being is the primary goal in aesthetic and reconstructive surgery. As a doctor, surgeon, or nurse, one always aims to provide the best possible treatment, recovery, and overall experience. By using compression after the procedure, pressure is applied to the operated area, which contributes to a better outcome. Compression can be administered in various forms, such as a girdle, bra, garment, or bandage.
In addition to providing support and stability, compression helps to improve the drainage of fluids from the tissue back into the circulation. This contributes to better healing and a reduced risk of swelling and complications, leading to a more comfortable and effective recovery. Compression is therefore a very important part of the rehabilitation process.

Fluid Accumulation and Swelling
Surgery can lead to fluid accumulation and swelling in the operated area, especially in procedures involving incisions in tissues or manipulation of blood vessels and lymphatic vessels. What happens when oxygen-rich blood enters the capillary on the arterial side can be explained using Starling's law, which describes the exchange of fluid across capillary walls.
A vessel rich in fluid exerts pressure against the capillary wall. Because there is less fluid outside the blood vessel, this pressure pushes fluid out to achieve equilibrium. This is called hydrostatic pressure (Pc) and promotes filtration. As fluid is pushed out of the blood vessel, the pressure decreases, and instead, pressure against the blood vessel increases. This pressure is called the interstitial hydrostatic pressure (Pi) and causes fluid to flow back into the blood vessel and be reabsorbed.
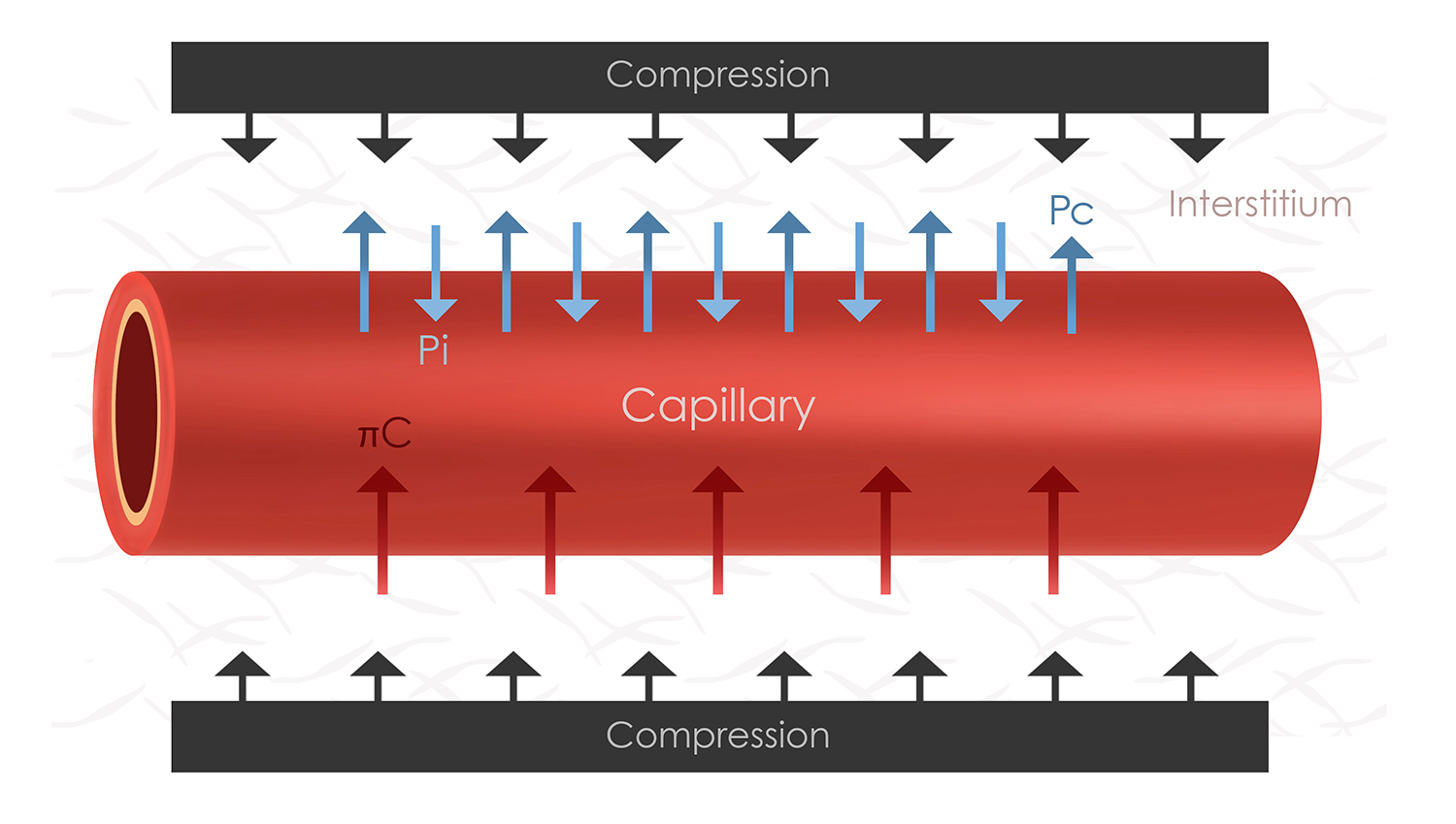
In addition to these two pressures, there is colloid osmotic pressure (πc). This is exerted by large proteins such as albumin and haptoglobin, which are always present in the blood. They draw fluid back into the blood vessel, helping to maintain fluid balance. After surgery, this pressure can decrease due to blood loss, resulting in diluted blood. Consequently, the blood contains fewer of these proteins, and fluid is not drawn back as effectively from the tissues. If the capillary wall also increases its permeability, which often occurs in conjunction with surrounding damaged tissue, this can lead to fluid accumulation and edema.
Increased Drainage with Compression
By applying external compression, a so-called mechanical pressure is created. This increases the pressure against the blood vessel and affects the flow of fluid in the venous blood vessels. This leads to improved venous return and lymphatic drainage. The pressure also promotes the absorption of fluid into the lymphatic vessels. The risk of excess fluid accumulating in the operated area is reduced by compressing blood vessels and lymphatic vessels.
Compression thus results in increased drainage of fluid, contributing to reduced fluid in the tissue and decreased swelling. The removal of waste products and carbon dioxide becomes more efficient, promoting the healing process and reducing the risk of infections and tissue necrosis. The support to the operated area reduces the strain on the damaged tissues. This contributes to reduced pain and better mobility during recovery. Improved mobility also decreases the risk of blood clots after surgery, making compression a valuable aid in reducing complications following surgical procedures. However, it is important to use compression correctly and under the supervision of medical personnel. For example, excessively high compression could restrict flow in superficial vessels and theoretically lead to necrosis.
In summary, compression contributes to:
• Reducing swelling and edema by draining excess fluid.
• Improving blood circulation by facilitating blood flow to and from the operated area.
• Providing support and stability to the tissues in the operated area.
• Reducing the risk of blood clots by improving venous return and decreasing venous stasis.
• Promoting wound healing through reduced swelling.

 Svenska
Svenska  Dansk
Dansk  Norsk
Norsk  Deutsch
Deutsch 



